With FPG Endovascular Surgeon James Shepherd, MD
Everyone knows that getting hairier is part of getting older, but getting veinier? Weird but true.
We’ve all seen it. The bright red capillaries at the end of the nose. The cord-like veins in the legs. As we age, the wear and tear on our circulatory system adds up. Spider veins are extremely common but roughly 3 in 10 adults will even develop varicose veins at some point. “And as long as they’re small, like spider veins, it’s purely cosmetic,” says Dr. James Shepherd. “But once you start noticing bulging veins that look like little ropes, those are varicose veins and there’s more going on.”
What are varicose veins?
Varicose veins are superficial veins that have become twisted and swollen, so that they stand out from the skin like squiggly purple or blue ropes. They can be a cosmetic concern, but they can also lead to uncomfortable symptoms and be a sign of a significant underlying condition known as chronic venous insufficiency.
Varicose veins appear most often in the legs but can occur elsewhere.
Did You Know?
Though most common in the legs, due to increased blood pressure, varicose veins can appear in many places. Hemorrhoids, for example, are varicose veins that develop in the rectum.
What causes varicose veins?
It’s estimated that the average human body has about 60,000 miles of arteries, veins and capillaries running through it—that’s more than enough to go around the world twice. And the heart is responsible for pumping blood through all of it. But it can’t do all the work alone.
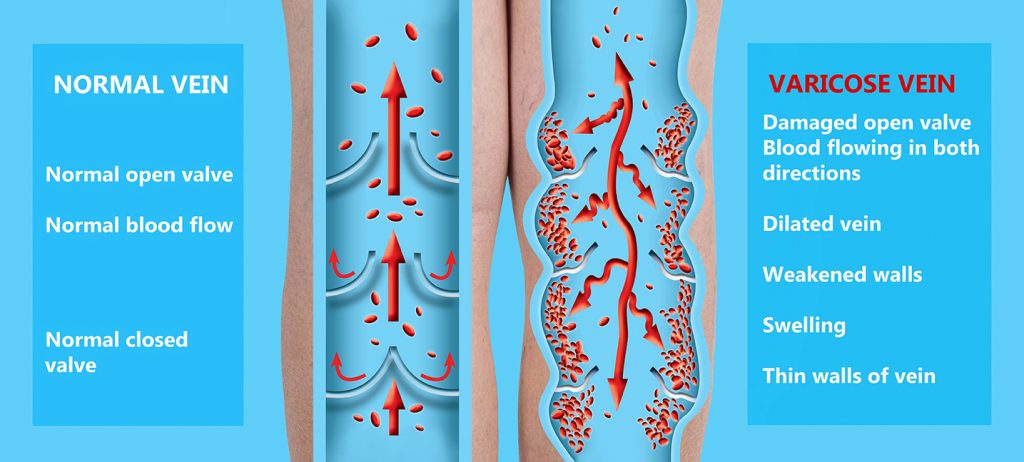
By the time blood reaches the tips of your toes and begins to make the trip back to the heart, it’s slowing down and fighting gravity, so muscles in your legs help the blood make the journey, contracting and squeezing the blood up toward the heart. Along the way, little valves in your veins act as stopgaps, closing between muscle contractions to keep the rising blood from falling back down to your feet.
But when those valves fail, and rising blood is continually allowed to fall back down and pool in the veins of the legs and feet, the increased pressure can damage the blood vessels and lead to varicose veins.
Other causes of increased blood pressure can also increase your chance of developing varicose veins. These include:
- Age
- Pregnancy
- Obesity
- Inactivity
- Sitting or standing for long periods of time
- Genetic history
What are the symptoms of varicose veins?
In addition to their visible appearance, varicose veins may also present with a variety of uncomfortable symptoms, including:
- Itching or burning around the affected veins
- Changes in skin color around the affected veins
- Swelling in legs
- Aches and pains in legs
- Heaviness in the legs and feet
- Nighttime leg cramps
- Worsened symptoms after periods of prolonged sitting or standing
If left untreated, varicose veins can lead to further complications, including uncontrolled bleeding, ulcers and edema.
How are varicose veins diagnosed?
Varicose veins are often diagnosed through a combination of physical exam and ultrasound imaging.
A simple visual inspection can be enough to confirm the presence of varicose veins, while a few questions about symptoms, lifestyle and family history can help point to a cause. An ultrasound provides detailed images of the affected veins, so the physician can plan appropriate treatment.
What is the treatment for varicose veins?
Treatment for varicose veins differs greatly, depending on the severity of symptoms and underlying conditions.
For mild cases, lifestyle changes may be recommended to alleviate symptoms or prevent varicose veins from worsening. These may include:
- Weight loss – A healthy weight keeps excess pressure off your veins.
- Regular physical activity – Staying physically active, particularly walking and other low-intensity cardio exercises, helps keep the blood flowing through your legs instead of pooling. However, intense exercise could make varicose veins worse, so consult with your doctor before jumping into a triathlon.
- Compression Hose – Also called compression stockings, these specially fitted socks are designed to improve blood flow and help relieve symptoms of varicose veins.
- Avoid standing or sitting for long periods – And when sitting, elevate your feet if possible.
- Quit smoking – Cigarettes and tobacco use harm vascular health, increasing risk of varicose veins
In other cases, treatment may be required to close off or even fully remove varicose veins.
- Sclerotherapy seals off the affected vein with a small injection. When the varicose vein seals shut and eventually fades away, blood flow is taken over by healthy veins. This procedure can be done in an outpatient visit with minimal side effects.
- Venous Sealing is a similar procedure for treating larger varicose veins. Entering the bloodstream at the ankle, a catheter is used to inject a medical adhesive foam that seals off the vein, while shunting blood flow to healthy veins. The procedure takes about 20-40 minutes and has minimal side effects.
- Endovenous ablation utilizes laser or radiofrequency energy to seal off varicose veins.
- Phlebectomy is a minimally invasive procedure by which smaller varicose veins are surgically removed.
For varicose veins that are larger and deeper, the physician may recommend vein ligation or “vein stripping,” which is surgical removal of the affected vein.

James Shepherd, MD, is a general surgeon with First Physicians Group. He specializes in vascular medicine. For more information or to make an appointment with Dr. Shepherd, please visit his profile.


